Achi news desk-
You may have heard of Ozempic, the “miracle drug” for weight loss, but did you know that it was actually designed as a new treatment to manage diabetes? In Canada, diabetes affects about 10 percent of the general population. Of those cases, 90 percent have Type 2 diabetes.
This metabolic disorder is characterized by persistently high blood sugar levels, which can come with secondary health challenges, including increased risk of stroke and kidney disease.
Locks and keys
In Type 2 diabetes, the body struggles to maintain blood sugar levels in an acceptable range. Every cell in the body needs sugar as a source of energy, but too much sugar can be toxic to cells. This equilibrium needs to be tightly managed and regulated by a lock and key system.
In the body’s attempt to control blood sugar levels and ensure that cells receive the right amount of energy, the pancreatic hormone, insulin, acts as key. Cells cover themselves with locks which responds perfectly to insulin keys to facilitate the entry of sugar into cells.
Unfortunately, this lock and key system does not always perform as expected. The body may face difficulties in producing a sufficient number of insulin keys, and/or the keys may become stubborn and unresponsive to insulin.
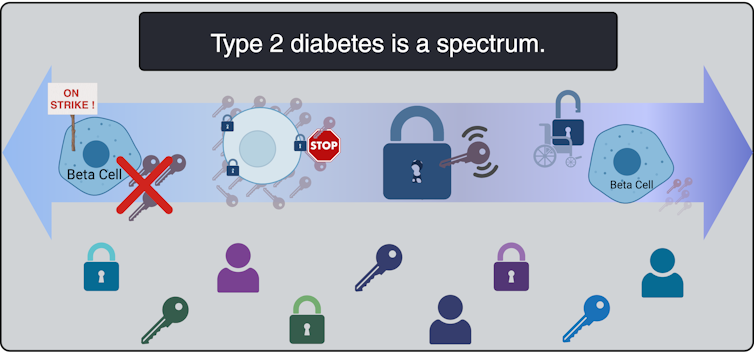
All types of diabetes share the challenge of high blood sugar levels; however, diabetes is not an individual condition; it exists as a spectrum. Although diabetes is broadly classified into two main types, Type 1 and Type 2, each presents with a variety of subtypes, particularly Type 2 diabetes.
These subtypes have their own characteristics and risks, and do not respond uniformly to the same treatments.
In order to better serve people living with Type 2 diabetes, and move away from a “one size fits all” approach, it is beneficial to understand which subtype of Type 2 diabetes a person is living with. When someone needs a blood transfusion, the medical team needs to know the patient’s blood type. It should be the same for diabetes so that an effective tailored game plan can be implemented.
This article examines four unique subtypes of Type 2 diabetes, shedding light on their causes, complications and some of their specific treatment pathways.
Severe insulin-deficient diabetes: Keys are missing!
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Insulin is produced by beta cells, which are found in the pancreas. In the severe insulin-deficient diabetes subtype (SIDD), the key factories – the beta cells – are on strike. Eventually, there are fewer keys in the body to unlock the cells and allow sugar to enter the blood.
SIDD mainly affects younger, slimmer individuals, and unfortunately, increases the risk of eye disease and blindness, among other complications. Why beta cells go on strike remains largely unknown, but since there is a lack of insulin, treatment often involves insulin injections.
Severe insulin-resistant diabetes: But it’s always locked!
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
In the severe insulin-resistant diabetes subtype (SIRD), the locks are overstimulated and begin to ignore the keys. As a result, the beta cells produce even more keys to compensate. This can be measured as high levels of insulin in the blood, also known as hyperinsulinaemia.
This insulin resistance is particularly pronounced in individuals with a higher body weight. Patients with SIRD have an increased risk of complications such as fatty liver disease. There are many treatment pathways for these patients but there is no consensus about the best possible approach; patients often require high doses of insulin.
Obesity-related mild diabetes: The locks are sticky!

(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Mild obesity-associated diabetes (MOD) is a subtle aspect of Type 2 diabetes, often seen in individuals with a higher body weight. Unlike more severe subtypes, MOD is characterized by a more moderate response to insulin. The locks are “sticky,” so it is challenging for the key to click into place and open the lock. Although MOD is associated with body weight, the relatively less severe nature of MOD distinguishes it from other diabetes subtypes.
To minimize complications, treatment should include maintaining a healthy diet, controlling body weight, and incorporating as much aerobic exercise as possible. This is where drugs such as Ozempig can be prescribed to control the evolution of the disease, in part by controlling body weight.
Mild age-related diabetes: I’m tired of controlling blood sugar!
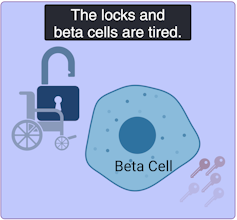
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Mild age-related diabetes (MARD) occurs more often in older people and usually starts later in life. With time, the key factory becomes less productive, and the locks become stubborn. People with MARD find it difficult to control their blood sugar, but it usually does not lead to serious complications.
Among the different subtypes of diabetes, MARD is the most common.
Unique locks, various keys
Although efforts have been made to classify diabetes subtypes, new subtypes are still being identified, making appropriate clinical assessment and treatment plans challenging.
In Canada, unique cases of Type 2 diabetes in aboriginal children from Northern Manitoba and Northwestern Ontario were identified by Dr. Heather Dean and colleagues in the 1980s and 90s. Despite initial skepticism from the scientific community, which usually associated Type 2 diabetes with adults rather than children, clinical teams continued to identify this as a distinct subtype of Type 2 diabetes, known as Type 2 diabetes beginning in childhood.
Read more:
Indigenous community research partnerships can help address health inequalities
Childhood onset Type 2 diabetes is on the rise across Canada, but it disproportionately affects Indigenous youth. It is undoubtedly related to the intergenerational trauma associated with colonization in these communities. Although many factors are likely to be involved, recent studies have found that fetal exposure to Type 2 diabetes during pregnancy increases the risk of the baby developing diabetes later in life.
The recognition of this particular subtype of Type 2 diabetes in First Nations communities has led to the implementation of a community health action plan aimed at addressing the unique challenges faced by Indigenous Peoples . It is hoped that research in partnership between communities and researchers will continue to help us understand childhood onset Type 2 diabetes and how to effectively prevent and treat it.
A mosaic of conditions
(Lili Grieco-St-Pierre, Jennifer Bruin/Created with BioRender.com)
Type 2 diabetes is not uniform; it is a mosaic of conditions, each with its own characteristics. Because diabetes is so unique in each patient, even categorization into subtypes does not guarantee how the disease will evolve. However, understanding these subtypes is a good starting point to help doctors create personalized plans for people living with the condition.
Although Indigenous communities, lower income households and individuals living with obesity already face a higher risk of developing Type 2 diabetes than the general population, tailored solutions may offer hope for better management. This emphasizes the urgent need for more precise assessments of diabetes subtypes to help adapt therapeutic strategies and management strategies. This will improve care for all patients, including those from vulnerable and understudied populations.
Ad blocking test (Why?)





Source link
Related

